In the intricate world of healthcare, clinical laboratory scientists (CLS) stand as the unsung heroes behind the scenes. These professionals, often referred to as medical laboratory scientists or technologists, are responsible for performing complex diagnostic tests that inform up to 70% of medical decisions. From analyzing blood samples for infectious diseases to identifying genetic markers for cancer, CLS ensures accuracy, timeliness, and reliability in results that directly impact patient outcomes. However, the demands on these scientists are intensifying: rising patient volumes, staffing shortages, and the need for rapid turnaround times (TAT) amid global health challenges like pandemics and aging populations.
Enter artificial intelligence (AI) and automation technologies that have sparked both excitement and apprehension in the clinical laboratory field. Automation, in the form of robotic systems and conveyor belts, has been streamlining workflows for decades, while AI, powered by machine learning (ML) and deep learning algorithms, is now analyzing vast datasets at speeds unattainable by humans. Yet, a common misconception persists: that these tools will render CLS obsolete. This couldn’t be further from the truth. As evidenced by numerous studies and real-world implementations, AI and automation are poised to enhance the role of CLS, allowing them to focus on high-level interpretation, quality assurance, and innovative problem-solving rather than repetitive tasks.
This article explores how AI and automation are transforming clinical laboratories by improving efficiency, accuracy, and patient care without displacing human expertise. Drawing from recent advancements and case studies, we’ll examine specific applications, benefits, challenges, and future prospects. Ultimately, these technologies act as collaborative partners, empowering CLS to deliver superior healthcare in an era of unprecedented demands.
The Evolution of Automation in Clinical Laboratories
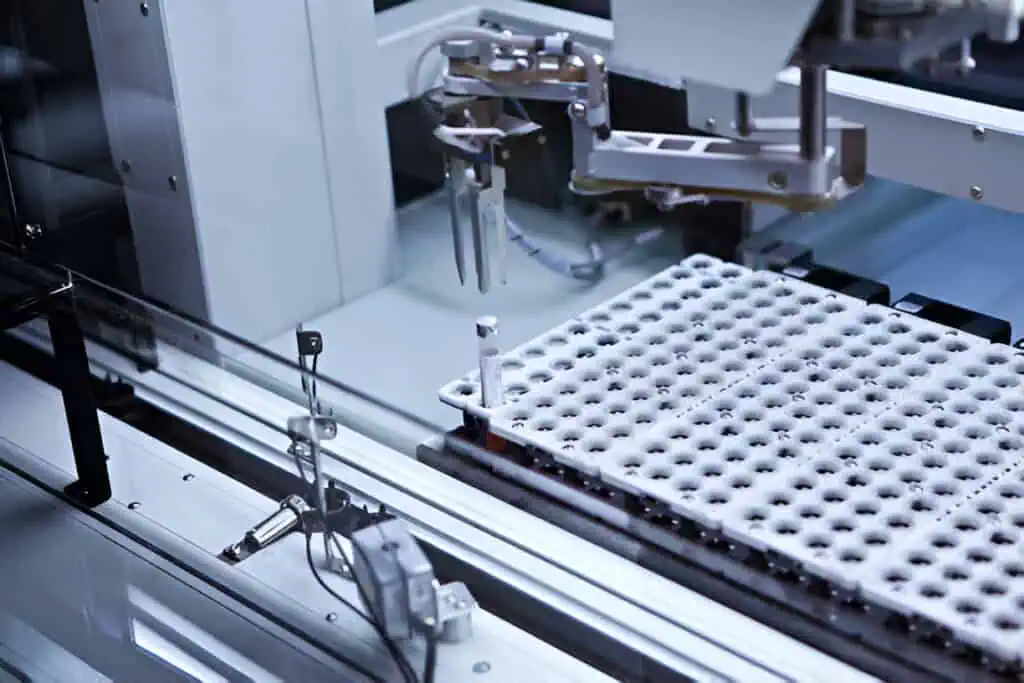
The journey toward automated clinical labs began in the mid-20th century with the introduction of basic analyzers for routine tests like glucose and cholesterol measurements. By the 1980s, automated instruments had become commonplace, reducing manual pipetting and minimizing errors in high-volume testing. However, true transformation arrived with total laboratory automation (TLA) systems in the 1990s and 2000s, integrated platforms that handle sample sorting, centrifugation, aliquoting, and analysis via robotic arms and track systems.
TLA represents a paradigm shift, consolidating disparate lab sections like hematology, chemistry, and immunology into unified workflows. For instance, systems from vendors like Siemens Healthineers or Roche Diagnostics can process thousands of samples daily with minimal human intervention. This evolution addresses longstanding issues: pre-automation labs often suffered from fragmented operations, where samples traveled between departments, leading to delays and contamination risks.
A compelling example comes from the Spedali Civili hospital in Brescia, Italy, where four separate labs were merged into a single Core-Lab in 2015 using TLA. Pre-merger, the labs operated with dedicated staff and equipment, resulting in variable TAT and higher costs. Post-implementation, automation led to a 12.55% reduction in total costs, primarily through staff optimization reducing overall personnel by 15% while extending services to 24/7 coverage. Equipment costs rose slightly due to new TLA infrastructure, but this was offset by eliminating redundant backup analyzers.
Critically, TAT improved for non-emergency tests, and emergency validations remained within hospital limits, demonstrating how automation enhances operational resilience without eliminating jobs. Instead, CLS were reassigned to oversight roles, ensuring system integrity and handling exceptions like anomalous results.
Automation also bolsters safety. Manual handling exposes staff to biohazards, but robotic systems minimize contact with samples, reducing accident rates. In one study, TLA improved productivity while addressing workforce shortages, allowing labs to manage increased volumes without proportional staffing hikes. This evolution underscores automation’s role as an enhancer: it frees CLS from mundane tasks, enabling them to engage in interpretive work that requires human judgment, such as correlating results with clinical histories.
AI Applications in Laboratory Medicine
Building on automation’s foundation, AI introduces cognitive capabilities that mimic human reasoning but scale exponentially. In clinical labs, AI encompasses ML algorithms for pattern recognition, natural language processing (NLP) for data extraction, and computer vision for image analysis. These tools integrate with laboratory information systems (LIS) to predict, detect, and interpret.
One primary application is in instrument automation and error detection. AI-powered analyzers, like those using neural networks for urine sediment analysis, classify particles with high accuracy, flagging anomalies for CLS review. Similarly, in hematology, AI automates cell counting and morphology assessment, identifying abnormalities like leukemia blasts faster than manual microscopy. The FDA has approved systems that enumerate erythrocytes, leukocytes, and platelets in blood and body fluids, reducing turnaround from hours to minutes.
In microbiology, AI enhances pathogen identification. For example, algorithms analyze mass spectrometry data from MALDI-TOF systems to detect bacteria in blood cultures within 24-48 hours, guiding antibiotic selection. AI-assisted image analysis detects mycobacteria or parasites in smears, a boon for resource-limited settings where CLS expertise is scarce. In pathology, convolutional neural networks (CNNs) scan digital slides for cancer markers, achieving diagnostic performance rivaling pathologists in tasks like lymph node metastasis detection.
Predictive analytics is another frontier. AI models forecast lab test values based on patient data, optimizing resource use and avoiding unnecessary tests. For instance, in patient blood management, AI predicts transfusion needs, reducing waste. Genomic analysis benefits from AI’s ability to sift through vast datasets, identifying mutations for personalized therapies. Tools like those from Mayo Clinic’s Computational Pathology and AI (CPAI) division use ML to recognize patterns in molecular data, aiding in acute myeloid leukemia prognosis.
Result interpretation and utilization management are also augmented. AI streamlines test ordering by suggesting appropriate panels based on symptoms, curbing overutilization. In emergency departments, AI triages samples by urgency, improving flow. These applications don’t replace CLS; they provide decision support, allowing scientists to validate AI outputs and integrate them with clinical context a uniquely human skill.
Benefits to Clinical Laboratory Scientists

The integration of AI and automation yields profound benefits for CLS, foremost among them enhanced efficiency and accuracy. Automation handles repetitive pipetting and sorting, slashing processing times by up to 50% in high-throughput labs. AI reduces human error in interpretation; studies show ML algorithms outperforming humans in image-based diagnoses for pneumonia or skin lesions, with error rates dropping below 5%. This accuracy is vital in critical sectors like oncology, where misreads can alter treatment paths.
By automating routine tasks, these technologies alleviate burnout, a pressing issue amid staffing shortages. CLS can redirect efforts to complex analyses, research, and patient consultation, fostering job satisfaction. In the Brescia case, staff reallocation supported growth without hires, improving morale. Cost savings follow: one review noted TLA leading to decreased workforce needs while boosting productivity.
Patient outcomes improve indirectly. Faster TAT enables timely interventions; AI’s predictive power in infectious disease testing accelerates antibiotic decisions, boosting cure rates. In low- and middle-income countries, AI bridges expertise gaps, empowering local CLS with global insights. Overall, these tools amplify CLS impact, transforming them from technicians to strategic diagnosticians.
Case Studies: Real-World Enhancements
Real-world deployments illustrate AI and automation’s enhanced role. At Mayo Clinic, the CPAI division integrates AI across labs for pattern recognition in imaging and molecular data. AI scans ECGs from wearables to detect weak heart pumps, aiding CLS in cardiovascular diagnostics. This has expanded research into personalized therapies without reducing staff roles.
Humber River Health in Canada, North America’s first fully digital hospital, uses AI for workflow optimization. Robotic systems handle sample transport, while AI predicts patient admissions via tools like POPP, allowing CLS to proactively allocate resources. This reduced emergency psychiatric admissions by 17% in related mental health initiatives.
HCA Healthcare partnered with Azra AI to automate oncology workflows. The platform analyzes pathology reports in real-time, identifying cancer cases and prioritizing reviews. This eliminated manual sifting, speeding diagnoses and enabling CLS to focus on validation, cutting delays in patient care.
The University of Rochester Medical Center (URMC) deployed Butterfly IQ probes with AI-enhanced imaging for students and clinicians. These handheld devices use ML for sharp diagnostics of conditions like cholecystitis, improving access and training. URMC plans to triple usage by 2026, enhancing CLS efficiency in point-of-care testing.
Valley Medical Center implemented Xsolis’ Dragonfly platform for AI-driven medical necessity scoring. This optimized observation rates, reallocating staff to high-priority cases, and boosting satisfaction. These cases show AI as a force multiplier, not a substitute.
Challenges and Ethical Considerations

Despite benefits, challenges persist. Data quality is paramount; biased or incomplete datasets can perpetuate inequities, as seen in algorithms favoring certain demographics. Privacy concerns arise with AI handling sensitive health data, necessitating robust regulations like HIPAA.
Implementation costs hardware, training, and integration, which can strain budgets, though long-term savings offset this. CLS requires upskilling; programs like those from ASCLS emphasize AI literacy to avoid over-reliance. Ethical dilemmas include AI’s “black box” nature, where decisions lack transparency, demanding human oversight.
Addressing these requires collaboration: labs must validate AI outputs, and policymakers must enforce standards. When managed, these hurdles ensure equitable enhancement.
Future Outlook
Looking ahead, AI and automation will deepen integration with LIS for seamless predictive analytics. Generative AI could create custom protocols, while ambient intelligence automates documentation. In personalized medicine, AI will tailor therapies based on genomics, with CLS interpreting nuances.
“Smart labs” will emerge, using AI for real-time optimization and sustainability. As adoption grows, CLS will evolve into AI-augmented experts, driving innovation in diagnostics and beyond.
Conclusion
AI and automation are revolutionizing clinical laboratories, but their true value lies in enhancement, not replacement. By streamlining workflows, boosting accuracy, and freeing CLS for meaningful work, these technologies elevate healthcare delivery. As we navigate challenges, the partnership between human ingenuity and machine intelligence promises a brighter future for patients and professionals alike.