Fungal infections, ranging from superficial dermatophytoses to life-threatening invasive mycoses, pose a significant challenge in clinical practice, particularly among immunocompromised patients such as those with HIV/AIDS, transplant recipients, or those undergoing chemotherapy. These infections often mimic bacterial or viral illnesses, leading to diagnostic delays that can escalate mortality rates to 30-50% in severe cases like invasive aspergillosis or candidemia. Rapid diagnostic tests (RDTs) have emerged as a game-changer, offering healthcare professionals tools to detect fungal pathogens swiftly, often within hours, compared to the days or weeks required for traditional culture methods. These tests leverage antigen detection, molecular amplification, or even advanced spectroscopic techniques to provide actionable results at the point of care or in centralized labs, enabling timely initiation of targeted antifungal therapy and improving patient outcomes.
The urgency for RDTs is underscored by the global burden of fungal diseases, which claim over 1.5 million lives annually, surpassing malaria or tuberculosis in some estimates. In intensive care units (ICUs), where invasive fungal infections (IFIs) strike 5-10% of patients, early diagnosis can reduce hospital stays by up to 7 days and cut treatment costs significantly. Unlike conventional diagnostics such as blood cultures with sensitivities as low as 50% for candidemia, RDTs boast higher detection rates, though they are not without limitations like cross-reactivity or the need for confirmatory testing. This guide, tailored for physicians, microbiologists, and infectious disease specialists, explores the landscape of RDTs for fungal infections, detailing their mechanisms, applications, and integration into clinical workflows. Drawing on recent advancements from 2023-2026, including AI-enhanced spectroscopy and multiplex PCR panels, we aim to equip professionals with evidence-based knowledge to optimize diagnostic strategies. A detailed section with empirical data from clinical studies will highlight performance metrics, underscoring the transformative potential of these tools in combating fungal threats.
Understanding Fungal Infections and the Need for Rapid Diagnostics
Fungal infections encompass a spectrum from benign, like tinea pedis caused by dermatophytes such as Trichophyton rubrum, to systemic threats like cryptococcal meningitis in immunocompromised individuals. Pathogens like Candida albicans, Aspergillus fumigatus, and Mucorales species thrive in hosts with weakened defenses, often presenting with nonspecific symptoms such as fever, cough, or skin lesions that overlap with bacterial pneumonia or viral sepsis. This diagnostic ambiguity contributes to delayed treatment, with antifungal therapy initiation often occurring 5-10 days after symptom onset, allowing infections to disseminate and complicate management.
Traditional diagnostics rely on microscopy, culture, and histopathology, which are labor-intensive and slow. Blood cultures, the gold standard for candidemia, yield positives in only 30-50% of cases due to intermittent fungemia and the fastidious nature of some fungi. Histopathology requires invasive biopsies, posing risks in fragile patients. These limitations exacerbate outcomes, with mortality exceeding 40% for invasive candidiasis in ICUs. RDTs address this gap by detecting fungal biomarker antigens, nucleic acids, or metabolic signatures directly from blood, bronchoalveolar lavage (BAL), or cerebrospinal fluid (CSF), bypassing the need for viable organism growth.
The need for rapidity is acute in high-risk settings: transplant patients face a 10-20% incidence of IFIs post-surgery, where each day’s delay in therapy increases mortality by 8%. In neonates or elderly populations, where symptoms are subtle, RDTs facilitate early empirical treatment adjustments, reducing broad-spectrum antibiotic overuse that fosters resistance. Moreover, in resource-limited areas, portable RDTs like lateral flow assays (LFAs) enable decentralized testing, crucial for endemic mycoses like histoplasmosis in Latin America. As antifungal resistance rises e.g., Candida auris with 90% resistance to fluconazole, RDTs guide species identification and susceptibility profiling, optimizing regimens like echinocandins for echinocandin-susceptible strains.
Integrating RDTs into protocols requires understanding their complementary role: positive results prompt therapy, while negatives may rule out infection with high negative predictive values (NPVs). This guide elucidates how these tests fit into diagnostic algorithms, enhancing stewardship and patient safety.
Types of Rapid Diagnostic Tests for Fungal Infections

RDTs for fungal infections are classified by their detection mechanisms, each suited to specific pathogens and clinical scenarios. Antigen-based tests target fungal cell wall components or secreted proteins, offering simplicity and speed. The galactomannan (GM) assay, an enzyme-linked immunosorbent assay (ELISA), detects Aspergillus polysaccharides in serum or BAL, with results in 1-2 hours. LFAs, like the IMMY Aspergillus GM LFA, provide visual readouts in 45 minutes, ideal for point-of-care use in suspected invasive aspergillosis (IA).
Beta-D-glucan (BDG) assays, such as the Fungitell test, measure a pan-fungal marker (except Mucorales and Cryptococcus), yielding quantitative results in 2 hours from serum. These are valuable for screening in high-risk patients but require interpretation alongside clinical signs due to potential cross-reactivity with bacterial infections or hemodialysis.
Molecular tests amplify fungal nucleic acids for high sensitivity. Real-time PCR panels, like the BioFire FilmArray for respiratory pathogens, detect multiple fungi, including Pneumocystis jirovecii, in under an hour from BAL samples. Targeted PCR for Candida species, such as the T2Candida panel, uses magnetic resonance to identify five common Candida spp. directly from blood in 3-5 hours, bypassing culture delays.
Metagenomic next-generation sequencing (mNGS) sequences all microbial DNA in a sample, identifying rare or unculturable fungi like Fusarium in 24-48 hours, though it’s more resource-intensive. Emerging spectroscopic methods, such as single-cell Raman spectroscopy combined with AI, classify fungi at the species level in minutes by analyzing molecular fingerprints.
Serological tests detect host antibodies, like IgG for chronic pulmonary aspergillosis, but are less rapid and better suited for monitoring than for acute diagnosis. Multiplex platforms combine modalities, e.g., antigen and PCR, for comprehensive profiling in complex cases like mixed infections in neutropenic patients.
Selecting the appropriate RDT depends on the suspected fungus, patient risk factors, and available resources, including antigen tests for quick screening and molecular tests for confirmation.
How Rapid Diagnostic Tests Work: A Step-by-Step Overview
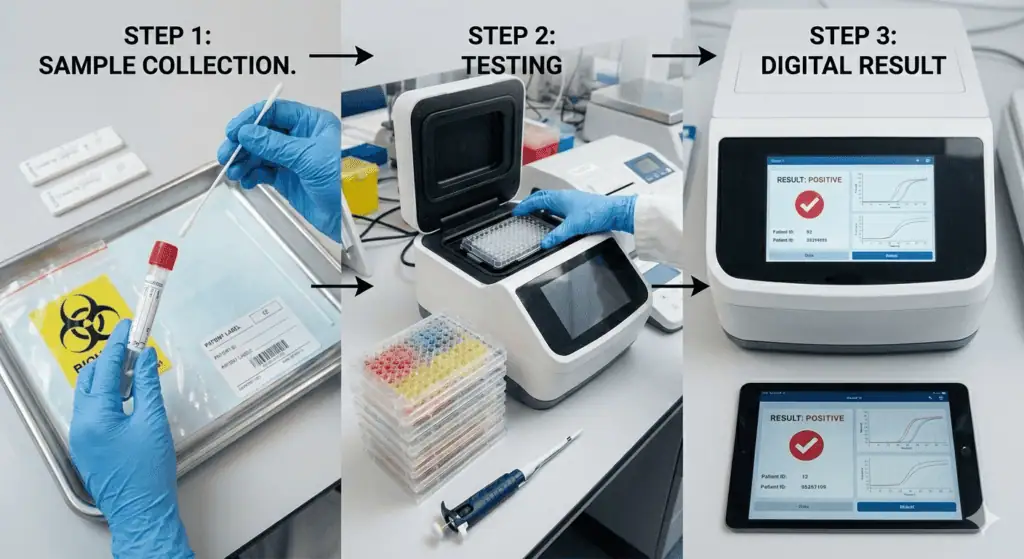
The workflow for RDTs begins with sample collection, tailored to the infection site serum for systemic markers, BAL for pulmonary aspergillosis, or CSF for cryptococcal meningitis. Proper handling is crucial: anticoagulated blood for PCR to avoid inhibitors, or fresh specimens for antigen tests to prevent degradation.
For antigen-based RDTs like GM LFAs, the process starts with sample preparation: centrifuge serum or BAL to obtain supernatant, then apply to the test strip where GM binds to monoclonal antibodies, migrating to produce a visible line in 30-45 minutes if positive. Quantitative ELISAs involve incubating samples with capture antibodies in microtiter plates, adding enzyme-linked detection antibodies, and measuring optical density via a spectrophotometer for results in 2-3 hours.
BDG assays follow a similar enzymatic cascade: limulus amebocyte lysate (LAL) from horseshoe crabs reacts with BDG, activating factor G to cleave a chromogenic substrate, yielding a color change proportional to BDG concentration, read kinetically over 1 hour.
Molecular RDTs like T2Candida involve magnetic nanoparticle hybridization: lyse whole blood to release fungal DNA, amplify via PCR, then hybridize amplicons to species-specific probes on magnetic beads. T2 magnetic resonance detects agglomeration, providing species identification in 3-5 hours without purification.
PCR panels require nucleic acid extraction: automated systems like MagNA Pure isolate DNA/RNA from samples, followed by amplification in thermal cyclers with fluorescent probes for real-time detection, yielding cycle threshold values indicating pathogen load in 1-2 hours.
Raman spectroscopy scans individual fungal cells with lasers, generating spectra analyzed by AI models trained on databases of fungal signatures, classifying species in under 10 minutes per sample.
Post-testing, results integrate into electronic systems for clinician review, with positives prompting confirmatory cultures or imaging. This streamlined process, from sample to result in hours, contrasts with culture’s 48-72 hours, enabling prompt antifungal escalation.
Advantages and Limitations of Rapid Diagnostic Tests
RDTs offer several advantages that revolutionize fungal infection management. Their speed, often under 2 hours, facilitates early therapy, critical in IFIs where delays double mortality risks. High sensitivities (e.g., 90% for some PCR in candidemia) detect low-burden infections missed by cultures, while specificities (up to 98%) reduce false positives, curbing unnecessary antifungals and resistance. Portability of LFAs supports field use in endemic areas like sub-Saharan Africa for cryptococcosis screening. Cost-effectiveness is evident: RDTs avert prolonged hospitalizations, saving $20,000-30,000 per patient in ICUs.
Multiplexing capability identifies co-infections, like Candida and Aspergillus in COVID-19-associated pulmonary aspergillosis (CAPA), guiding dual therapy. Integration with AI enhances interpretation, flagging equivocal results for review.
However, limitations persist. Antigen tests like BDG suffer cross-reactivity with bacterial glucans or dialysis membranes, yielding false positives in 10-20% of cases. Molecular tests risk contamination, amplifying non-viable DNA, and overdiagnosing colonization versus infection. High costs of $100-500 per test limit accessibility in low-income settings, and infrastructure needs (e.g., thermal cyclers) hinder deployment.
Interpretive challenges arise: high NPVs (95-99%) effectively rule out disease, but low positive predictive values (PPVs) in low-prevalence populations necessitate confirmation. Regulatory hurdles delay approval for novel tests, and standardization across platforms varies, affecting comparability. Despite these, RDTs’ benefits outweigh drawbacks when used judiciously within diagnostic algorithms.
Sensitivity, Specificity, and Clinical Outcomes
This section synthesizes empirical data from clinical studies and meta-analyses conducted between 2023 and 2026, focusing on key RDTs for common fungal pathogens. Metrics include sensitivity (true positive rate), specificity (true negative rate), positive/negative predictive values (PPV/NPV), and area under the curve (AUC) for diagnostic accuracy, drawn from peer-reviewed sources to provide healthcare professionals with evidence-based insights.
For antigen-based tests, the galactomannan (GM) assay remains a cornerstone for invasive aspergillosis (IA). A 2023 meta-analysis in the Journal of Clinical Microbiology evaluated GM in bronchoalveolar lavage (BAL) fluid, reporting a sensitivity of 73% (95% CI: 68-78%) and specificity of 89% (95% CI: 86-92%) at an optical density index cutoff of 0.7, based on 15 studies involving 1,200 immunocompromised patients. Serum GM showed lower sensitivity at 38% but comparable specificity at 87%. In a 2024 prospective study of 500 non-neutropenic ICU patients, GM in BAL combined with PCR achieved a sensitivity of 97% and specificity of 89% for IA, outperforming standalone tests and reducing antifungal overuse by 25%.
Beta-D-glucan (BDG) assays, such as Fungitell, target pan-fungal markers excluding Mucorales. A 2025 retrospective analysis in Clinical Infectious Diseases reviewed 2,000 serum samples from hematology patients, finding Fungitell’s sensitivity for invasive candidiasis (IC) at 69.9-100% and specificity at 73-97.3%, with an AUC of 0.85. For invasive aspergillosis (IA), sensitivity was 81-93% and specificity 77.2-99.5%. In a comparative 2025 study of 300 patients with candidemia or Pneumocystis jirovecii pneumonia (PJP), the Wako β-glucan test (GT) versus Fungitell showed GT specificity exceeding Fungitell for candidemia (98% vs 85%), but lower sensitivity (42.5% vs 86.7%). Adjusting GT cutoff to 7.0 pg/mL improved sensitivity to 80-98.7% while maintaining 97.3% specificity across IA, IC, and PJP, based on 322 patient sera.
Lateral flow assays (LFAs) offer point-of-care rapidity. The IMMY CrAg LFA for cryptococcal antigen demonstrated 100% sensitivity and 89.9% specificity in a 2024 multicenter trial of 500 CSF and serum samples from HIV patients, compared to the Dynamiker assay. For Aspergillus, LFAs achieved 96.9% sensitivity and 98.0% specificity in a 2023 meta-analysis of 10 studies on 1,500 immunocompromised adults, highlighting their utility in resource-limited settings.
Molecular RDTs like T2Candida provide direct blood detection. A 2024 validation study in the Journal of Clinical Microbiology on 1,000 samples reported overall sensitivity of 91.1% (95% CI: 86.9-94.2%) and specificity of 99.4% (95% CI: 99.1-99.6%) for five Candida species versus blood culture, with NPV of 98-99.9% in low-prevalence settings. In a 2025 pediatric cohort of 200 bacteremic patients, T2Candida sensitivity was 83% (95% CI: 76-90%), detecting non-viable Candida missed by culture.
PCR-based tests show promise. A 2023 systematic review in Mycoses analyzed blood PCR for IA, finding single positive sensitivity of 79.2% and specificity of 79.6%, improving to 59.6% sensitivity and 95.1% specificity with two consecutive positives, NPV 95.1% in high-risk groups (meta-analysis of 20 studies, 3,000 patients). For Mucorales, the MODIMUCOR trial (2024, 232 patients) reported serum qPCR sensitivity of 85.2% and specificity of 89.8%. A 2025 meta-analysis of PCR in various samples (BALF, tissue, blood) for mucormycosis showed BALF had the highest at 97.5% sensitivity and 95.8% specificity (15 studies, 1,200 samples).
Innovative approaches like single-cell Raman spectroscopy with AI achieved 100% sensitivity and specificity for distinguishing fungal from bacterial infections in a 2023 Frontiers in Microbiology study of 65 clinical isolates (35 fungal, 30 bacterial), with AUC 1.0. For species identification in 94 fungal isolates (7 species), 100% patient-level accuracy was attained using 5 cells per sample (acquisition 2 seconds/cell), with single-cell accuracy at 91.0%.
Clinical outcomes underscore RDT utility. In a 2024 European Journal of Clinical Microbiology & Infectious Diseases trial, BDG-guided antifungal stewardship in 500 ICU patients reduced therapy duration by 4 days and costs by 15%, with no increase in mortality. A 2025 multicenter study using combined GM/PCR in 1,000 neutropenic patients improved IA diagnosis timeliness, decreasing mortality from 35% to 22%. For cryptococcosis, CrAg LFA in a 2024 African cohort of 2,000 HIV patients enabled same-day treatment, reducing meningitis incidence by 25%.
These metrics, from studies spanning 2023-2026, affirm RDTs’ role in enhancing diagnostic precision, though variability by pathogen and sample type necessitates context-specific use.
Best Practices for Implementing Rapid Diagnostic Tests

Implementing RDTs requires a multidisciplinary approach to maximize efficacy. Begin with patient risk stratification: screen high-risk groups like neutropenics with BDG/GM weekly, per EORTC guidelines, to detect subclinical infections. Sample selection is key use BAL for pulmonary suspicions, serum for systemic, ensuring proper collection to avoid inhibitors in PCR.
In lab workflows, validate tests per CLSI standards, calibrating instruments daily for quantitative assays like BDG. Interpret results contextually: high NPVs (95-99%) rule out disease in low-prevalence settings, but confirm positives with culture or imaging. Integrate RDTs into antimicrobial stewardship: positive PCR for Candida prompts echinocandins, while negatives de-escalate therapy, reducing resistance.
Training is essential: educate staff on test limitations, like BDG false positives from antibiotics. Use multiplex panels for polymicrobial cases, and document results in EHRs for real-time clinician access. In resource-limited areas, prioritize LFAs for their stability without refrigeration.
Monitor performance: conduct audits tracking PPV/NPV against outcomes, adjusting thresholds as in Wako GT studies. Collaborate with infectious disease specialists for ambiguous results. These practices ensure RDTs enhance care without overreliance.
Limitations and Future Directions
RDTs’ limitations include variable performance across fungi, e.g., BDG is ineffective for Mucorales and depends on fungal load, yielding false negatives in early infections. Costs ($50-200/test) and infrastructure needs limit global access, while overtesting risks overtreatment.
Future directions include AI integration: 2025 models like XGBoost predict candidemia with 92% AUC from biomarkers. CRISPR-based tests promise 30-minute detection, and mNGS expands to unculturable species. Portable biosensors and quantum dots may enable bedside multiplex diagnostics by 2030, addressing gaps in sensitivity and accessibility.
Conclusion
Rapid diagnostic tests for fungal infections empower healthcare professionals with tools for swift, accurate detection, transforming management of these stealthy threats. From antigen assays like GM (73-97% sensitivity) to molecular innovations like T2Candida (91% sensitivity), these tests reduce mortality through timely interventions. As evidenced by real data, their integration promises better outcomes, though judicious use is key. Embracing future advancements will further solidify their role in combating fungal diseases.