In an era where medical advancements promise longer, healthier lives, a stark reality persists: not everyone benefits equally. Health equity, defined by the Centers for Disease Control and Prevention (CDC) as the state where everyone has a fair and just opportunity to attain their highest level of health, remains elusive for many. This requires addressing historical injustices, economic barriers, and systemic biases that perpetuate health disparities and differences in health outcomes, adversely affecting socially disadvantaged groups. These disparities manifest in higher rates of chronic diseases, delayed diagnoses, and poorer treatment outcomes among racial and ethnic minorities, low-income populations, rural residents, and other marginalized communities.
Clinical laboratory science (CLS), the backbone of modern diagnostics, plays a pivotal role in bridging this gap. CLS encompasses the analysis of biological specimens to detect, diagnose, and monitor diseases, influencing an estimated 60-70% of all clinical decisions. From blood tests revealing diabetes to genetic screenings identifying cancer risks, lab results provide objective data that guides healthcare providers. Yet, the field itself faces inequities: limited access to testing in underserved areas, biases in diagnostic algorithms, and underrepresentation in the workforce. Despite these challenges, CLS is driving health equity through innovations like point-of-care testing, AI-enhanced diagnostics, and community-based initiatives.
This article explores how CLS addresses health disparities, drawing on statistics, real-world examples, and emerging technologies. By ensuring accurate, timely, and accessible diagnostics, CLS not only closes gaps in care but also empowers equitable health outcomes. As global health spending on in vitro diagnostics reaches $135 billion by 2030, the focus must shift to inclusive practices that benefit all. Ultimately, CLS is not just a scientific discipline; it’s a catalyst for social justice in healthcare.
Understanding Health Disparities: The Scope of the Problem
Health disparities are deeply rooted in social determinants of health (SDOH), including poverty, education, housing, and access to care. According to the Kaiser Family Foundation (KFF), Black, Hispanic, Native Hawaiian and Pacific Islander (NHPI), and American Indian and Alaska Native (AIAN) people are more likely than White individuals to be diagnosed with HIV or AIDS, with rates up to eight times higher in some groups.
Cancer disparities are equally alarming: the National Cancer Institute reports that African Americans have the highest death rates from most cancers, with prostate cancer mortality twice that of White men. Maternal health inequities highlight the crisis, where Black women in the U.S. face maternal mortality rates three to four times higher than White women, often due to undiagnosed conditions like preeclampsia.
Diagnostic disparities exacerbate these issues. A 2024 JAMA Network Open study found that racial and ethnic minorities in acute care settings receive lower rates of diagnostic testing, leading to missed opportunities for early intervention. For instance, in prostate cancer, inequities in multiparametric MRI (mpMRI) utilization mean underrepresented groups miss out on precise diagnostics, resulting in delayed treatments. Globally, the World Health Organization (WHO) notes that diagnostics influence 70% of healthcare decisions, yet only 3-5% of budgets are allocated to them, widening gaps in low-resource settings.
Socioeconomic factors compound this: low-income households report diagnostic problems and persisting harms at rates 1.5 times higher than affluent ones, per a 2025 PMC study. Gender and age biases also play a role; women and older adults often face underdiagnosis of conditions like heart disease due to atypical presentations overlooked in standard testing protocols. In mental health, individuals with conditions are at higher risk of diagnostic inequalities in physical healthcare, as evidenced by a 2024 Lancet study reviewing delayed diagnoses for comorbidities.
These statistics underscore a systemic failure: without equitable diagnostics, disparities persist. CLS emerges as a key player, providing the data needed to identify at-risk populations and tailor interventions.
The Core Role of Clinical Laboratory Science in Promoting Equity

At its heart, CLS ensures that diagnostics are accurate, accessible, and actionable. Medical laboratory scientists (MLS) perform complex analyses in areas like clinical chemistry, hematology, microbiology, and molecular diagnostics, using sophisticated equipment to process samples. This data supports patient-centered care, reducing errors and improving outcomes.
One way CLS drives equity is through stewardship of patient safety. The American Society for Clinical Laboratory Science (ASCLS) emphasizes that MLS professionals are key to multi-disciplinary teams, consulting on test selection and interpretation to avoid misdiagnoses. For example, in value-based care models, labs use data to inform health equity strategies, as seen in Labcorp’s initiatives, where lab insights help design care models for underserved populations.
Laboratory equity, providing affordable, timely diagnostic services, is crucial. A 2024 PMC article on clinical microbiology highlights how equitable lab access reduces disparities in infectious disease management. In public health, labs track outbreaks and monitor threats, as demonstrated during COVID-19, where testing disparities led to higher infection rates in minority communities.
Diversity in the CLS workforce is another driver. The Association for Diagnostics & Laboratory Medicine (ADLM) promotes equity through its Health Equity and Access Division, advocating for inclusive practices. Underrepresentation only 11% of lab professionals being Black, per workforce studies, mirrors broader disparities, but initiatives like ASCP’s studies propose introducing CLS careers to elementary students to build a diverse pipeline.
Moreover, CLS addresses biases in algorithms. A 2022 ADLM article discusses how lab data in estimating equations can perpetuate disparities if not adjusted for race, prompting calls for race-neutral formulas in kidney function tests. By refining these tools, CLS ensures equitable diagnostics.
Innovations in Clinical Laboratory Science: Tools for Equity

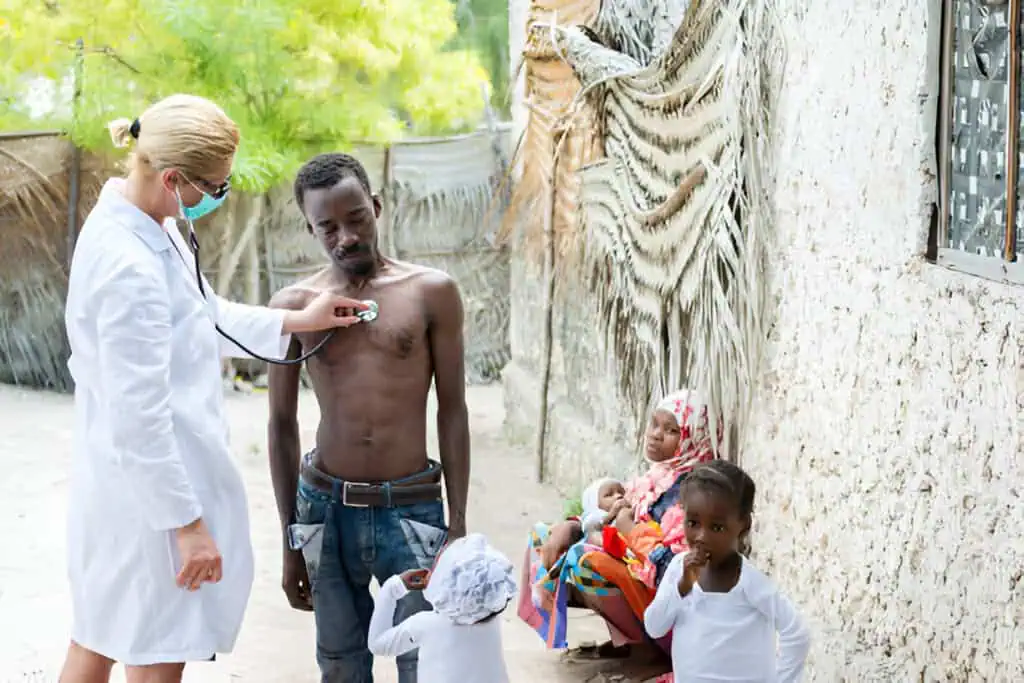
Technological advancements in CLS are revolutionizing access and accuracy. Point-of-care testing (POCT) allows rapid diagnostics in remote or underserved areas, bypassing traditional lab delays. For instance, mobile clinics equipped with POCT have brought testing to socioeconomically challenged communities, reducing barriers to care.
Artificial intelligence (AI) and machine learning enhance equity by analyzing vast datasets to detect patterns overlooked by humans. A 2021 JAMA Health Forum article notes AI’s potential to reduce diagnostic errors linked to disparities. Labcorp’s AI-enhanced Test Finder integrates into EHRs, enabling intuitive searches at the point of care. In precision medicine, next-generation sequencing (NGS) tailors treatments to genetic profiles, addressing disparities in conditions like breast cancer, where models from NIMHD’s Health Equity and Decision Sciences Lab support equitable care.
Telehealth-integrated labs extend reach: during the pandemic, remote sample collection and digital results reduced inequities. Big data analytics, as in Labcorp’s collaborations, use lab data to inform equity models. Innovations like 5G networks and smartphones enable real-time diagnostics in low-resource settings.
The WHO’s Essential Diagnostics List (EDL) guides equitable implementation, prioritizing tests for high-burden diseases. Automation trends for 2025, per CLP Magazine, predict AI dominating labs, improving efficiency, and reducing costs for disparate populations.
Case Studies: Real-World Impact
Real-world applications illustrate CLS’s equity-driving power. In maternal health, Sutter Health’s Health Equity Innovation Lab uses lab data to address childbirth inequities, reducing disparities in prenatal testing. For example, enhanced screening for gestational diabetes in Black and Hispanic women has lowered complication rates.
During COVID-19, lab innovations like rapid antigen tests mitigated disparities, though initial shortages highlighted gaps. In Rhode Island, state labs ensured equal access to quality testing, per a 2016 report.
Cancer screening programs exemplify success: ADLM’s efforts in eliminating disparities through lab-driven protocols have improved colorectal cancer detection in underrepresented groups. UC Berkeley’s pilots reduced racial gaps in breast cancer testing via innovative lab collaborations.
In cardiology, disparities in diagnosis are addressed through equitable use of biomarkers, as noted in a 2024 Canadian Journal of Cardiology review. These cases show CLS’s tangible role in saving lives and reducing inequities.
Challenges and Pathways Forward

Despite progress, challenges persist. Workforce shortages project 24,200 annual openings for MLS per the BLS, and limited capacity in underserved areas. Biases in diagnostics, like race-based adjustments, perpetuate harm. Access issues, including language barriers in patient portals, affect LEP patients.
Solutions include policy reforms: the NAM’s workshop on equity in diagnostics calls for inclusive research. Training in cultural competency, as per ASCLS, enhances care. Collaborative models like LAB-CARES streamline value-based care.
Future Directions: Toward Inclusive Diagnostics
Looking ahead, CLS must integrate health justice frameworks, as in Lurie Children’s I+HEAL lab, which uses implementation science for equitable pediatric care. Emerging trends like DCLS professionals will bridge labs and clinics. Global standards, per IFCC’s TF-OSLM, will document lab impacts.
Conclusion
Clinical laboratory science is indispensable in closing health equity gaps, providing the diagnostic foundation for fair care. By embracing innovations, addressing challenges, and prioritizing inclusivity, CLS can transform healthcare. Stakeholders must invest in this field to ensure no one is left behind. Health equity starts in the lab.