In the bustling corridors of a modern clinical laboratory, where automated analyzers hum and technicians peer into microscopes, the future of healthcare is being shaped one test at a time.
Precision medicine, an approach that tailors treatments to individual patients based on their genetic makeup, lifestyle, and environment, doesn’t begin in the doctor’s office or the operating room—it starts here, in the lab. As the FDA defines it, precision medicine is “an innovative approach to tailoring disease prevention and treatment that takes into account differences in people’s genes, environments, and lifestyles.” This paradigm shift has transformed healthcare from a one-size-fits-all model to a highly personalized strategy, potentially saving lives and reducing costs. According to a 2023 report, precision medicine could generate up to $1.2 trillion in value for the U.S. healthcare system by 2040 through improved outcomes and efficiency.
Yet, the lab’s role is often underappreciated. Laboratories provide the foundational data—genomic sequences, biomarker profiles, and molecular insights—that enable clinicians to make informed decisions. Without accurate, timely lab results, precision medicine remains an abstract concept. This article explores how labs are the epicenter of precision medicine, delving into key technologies, real-world case studies, challenges, and future directions. By examining these facets, we uncover how lab innovations are not just supporting but driving the evolution of personalized care.
Defining Precision Medicine and the Lab’s Foundational Role
Precision medicine, sometimes interchangeably called personalized medicine, emerged prominently in the early 2000s with advances in genomics following the Human Genome Project. It aims to deliver the “five rights”: the right patient, the right drug, the right time, the right dose, and the right route. At its core, this requires detailed biological data, much of which originates from laboratory testing.
Labs contribute through genetic testing and data analysis, which inform everything from cancer therapies to pharmacogenomics. For instance, genetic tests identify mutations that predict drug responses, preventing adverse reactions that affect millions annually. In the era of big data, labs integrate genomic information with environmental and social factors to enhance patient outcomes. Clinical laboratories have risen in prominence, with professionals playing a key role in interpreting complex data for precision approaches.
The definition of “normal” lab values is crucial, as it governs diagnosis and management. Variations in these values can lead to misdiagnoses if not personalized, highlighting the need for labs to adapt to individual baselines. Organizations like Precision for Medicine emphasize incorporating lab expertise with clinical trials and data intelligence to uncover patient biology insights. As one expert notes, “Precision medicine provides a biological approach to treatment that considers a patient’s genomic information.”
In practice, labs handle vast datasets. For example, next-generation sequencing (NGS) in labs sequences entire genomes rapidly, identifying variants linked to diseases. This data feeds into electronic health records (EHRs), enabling real-time personalization. Without labs, precision medicine would lack the empirical foundation to move from theory to therapy.
Key Technologies in Labs Driving Precision Medicine
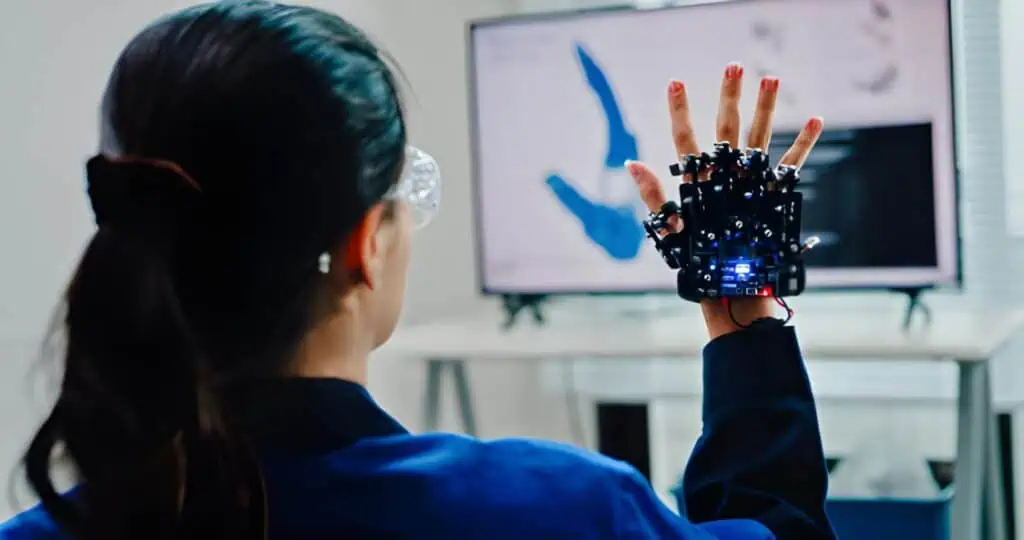
Laboratories employ cutting-edge technologies to fuel precision medicine, from molecular diagnostics to artificial intelligence (AI). These tools enable the analysis of complex biological systems at unprecedented scales.
One cornerstone is NGS, which allows labs to sequence DNA and RNA quickly and cost-effectively. NGS identifies genetic mutations, gene expressions, and epigenetic changes, essential for tailoring treatments in oncology and rare diseases. Paired with CRISPR-based diagnostics, labs can edit genes for functional studies or develop targeted therapies.
Liquid biopsies represent another breakthrough. These non-invasive tests analyze circulating tumor DNA (ctDNA) in blood, detecting cancers early and monitoring treatment responses without biopsies. In 2023, liquid biopsies topped the list of precision medicine technologies, offering real-time insights into tumor dynamics.
Microfluidics and lab-on-a-chip devices miniaturize assays, enabling point-of-care testing with minimal samples. These “labs in miniature” process fluids at microliter scales, accelerating diagnostics for remote or resource-limited settings. Flow cytometry, another key tool, sorts and analyzes cells based on biomarkers, aiding in immunotherapy development.
AI and machine learning integrate lab data with big data analytics. AI algorithms predict disease risks from genomic data, optimize drug dosing, and identify patterns in vast datasets. For instance, cloud platforms like Azure enable labs to store and analyze petabytes of data, facilitating collaborative precision efforts. Mass spectrometry (MS) provides detailed proteomic profiles, revealing protein interactions crucial for drug targeting.
Pharmacogenomics testing in labs assesses how genes affect drug metabolism, preventing inefficacy or toxicity. Tests for genes like CYP2D6 guide dosing for antidepressants and painkillers. Spatial technologies map molecular distributions in tissues, enhancing understanding of disease microenvironments. These technologies collectively empower labs to translate raw data into actionable insights.

Case Studies: Labs in Action for Precision Medicine
Real-world applications illustrate the lab’s pivotal role. In oncology, Memorial Sloan Kettering Cancer Center (MSKCC) has implemented precision oncology over a decade, using lab-based genomic profiling to match patients with targeted therapies. One case involved sequencing over 10,000 tumors, identifying actionable mutations in 37% of patients, leading to novel treatments and improved survival rates.
In drug development, Precision for Medicine supported concurrent Phase 1 trials for solid tumors. Labs provided biomarker analysis and central lab services, enabling adaptive designs that accelerated approvals. Another Phase 1-2 oncology study used lab data to monitor safety, resulting in proactive adjustments and successful outcomes.
For rare diseases, the University of Utah’s examples include molecular profiling to grow replacement tissues or find proper drug doses. In one scenario, lab genomics identified a genetic variant causing a child’s epilepsy, leading to a targeted antiepileptic drug that controlled seizures.
LabCorp’s case studies show bone void fillers tested in labs for regeneration potential, advancing orthopedic precision medicine. Acobiom’s collaborations used lab expertise to discover biomarkers for diagnostics in precision medicine. In real-world evidence, Geisinger’s clinico-genomic database integrated lab data with EHRs, informing population-level precision strategies.
From X (formerly Twitter), recent posts highlight ongoing lab work: Caris Life Sciences showcased their R&D lab advancing precision through innovation, while Gene Solutions launched a genomics lab in India to expand access. These examples demonstrate labs’ tangible impact on patient lives.
Challenges in Lab-Based Precision Medicine
Despite progress, challenges persist. High costs limit access; genomic sequencing can exceed $1,000 per test, exacerbating disparities in low- and middle-income countries (LMICs). Ethical issues, including data privacy and consent for genetic information, raise concerns.
Data fragmentation is rampant, with siloed systems causing duplication and inconsistencies. Integrating lab data with EHRs requires standardization, but variations in quality and formats hinder this. Precision trials face unique logistics: complex sample handling, multiple vendors, and disconnected systems complicate workflows.
Workforce shortages and inadequate training in LMICs impede adoption, alongside limited technology. Biomarker strategies struggle with funding and access, delaying therapies. Societal challenges include merging platforms and ensuring equity. Overcoming these demands requires investment in interoperability, education, and policy reforms.

Future Directions for Labs in Precision Medicine
By 2030, precision medicine could transform healthcare through seven key ways, including widespread genomics and AI integration. Labs will evolve, incorporating complex algorithms, digital health apps, and omics-based tests.
AI will power precision health, analyzing lab data for predictive models. Flexible lab designs will support rapid innovations, like modular facilities for diagnostics. In Wisconsin, companies like Accuray are pioneering radiation therapies guided by lab precision.
Global efforts will focus on equity, with AI addressing barriers in drug development. The market could reach $2.8 trillion by 2030, but bridging discovery to clinic remains key. Labs will lead in reshaping delivery, enhancing patient-specific treatments.
Conclusion
Precision medicine undeniably starts in the lab, where data becomes destiny. From genomic insights to AI-driven predictions, labs provide the tools to personalize care, as evidenced by case studies and technologies. While challenges like cost and data issues loom, the future promises equitable, transformative healthcare. Investing in labs isn’t just scientific—it’s a commitment to human potential.














