Live Blood Test Analysis offers a fascinating real-time window into the living dynamics of your blood. With just a single drop placed on a glass slide under a high-powered dark-field microscope, a vibrant world comes to life; red blood cells glide smoothly, white cells patrol for invaders, and platelets gather at microscopic injuries. Unlike traditional hematology, which fixes and stains samples for static observation, live blood test analysis examines fresh, unstained capillary blood within minutes of collection. This approach captures cellular activity, shape, and interactions as they naturally occur inside the body, offering unique insights into your overall health and microenvironment.
In 2025, over 45,000 practitioners worldwide, primarily naturopaths, functional medicine doctors, and integrative health coaches, will incorporate live blood test analysis into wellness assessments, with the global dark-field microscopy market valued at $185 million (Allied Market Research). While mainstream laboratories dismiss it as non-standardized, proponents cite immediate visual feedback that motivates lifestyle changes and detects subtle imbalances before they manifest in routine panels. This in-depth guide demystifies live blood test analysis: its procedural steps, observable markers, evidence-based benefits, accuracy benchmarks against gold standards, clinical integration pathways, regulatory status, ethical considerations, and emerging AI-enhanced protocols shaping its future.
Defining Live Blood Test Analysis: Principles and Procedural Workflow
Live blood test analysis involves examining a fresh capillary blood sample under phase-contrast or dark-field microscopy at 400x-1,000x magnification within 20 minutes of collection to preserve cellular viability. Oxygen, pH, and temperature remain near physiological levels, allowing observation of rouleaux formation, erythrocyte aggregation, fibrin strands, and microbial activity in real time.
The standardized protocol, as outlined by the International Association of Live Blood Analysts (IALBA), includes eight steps. First, the practitioner cleans the fingertip with 70% isopropyl alcohol and uses a sterile lancet for a 2-3 mm puncture. Second, the first drop is wiped away to minimize tissue fluid contamination. Third, a 2 µL droplet is transferred to a coverslip-mounted slide without anticoagulants or stains.
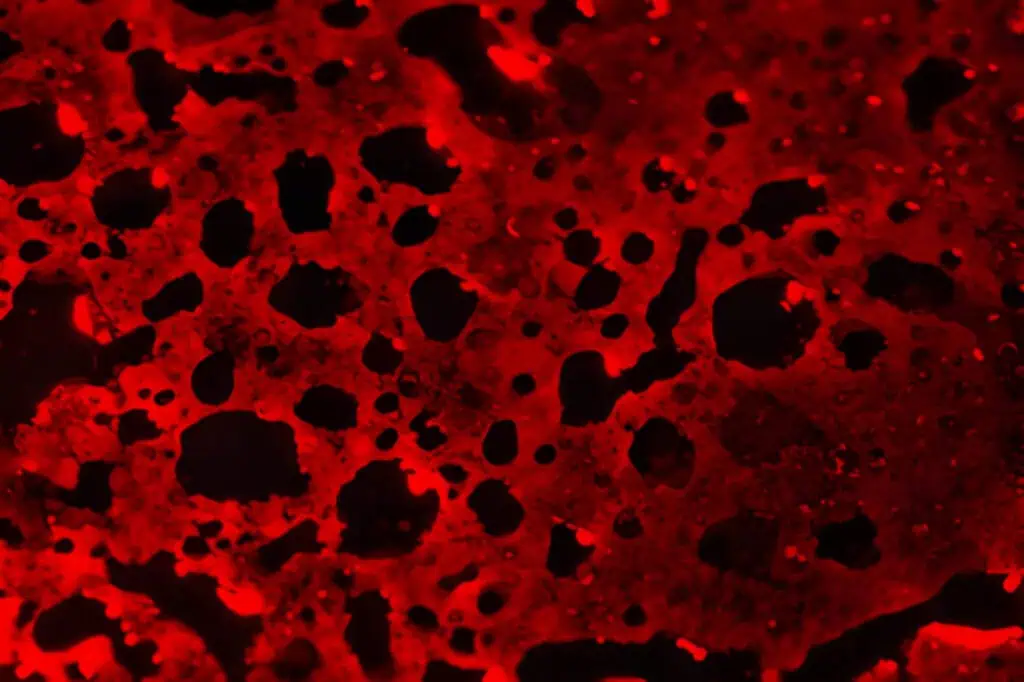
Fourth, the slide enters a preheated microscope stage at 37°C. Fifth, scanning begins in dark-field mode, where light scatters off cellular edges, creating a luminous halo against a black background. Sixth, digital capture via CMOS cameras records 60-second loops at 30 fps. Seventh, the practitioner narrates findings to the patient in real time. Eighth, a post-session report compiles annotated images with nutritional or lifestyle recommendations.
Equipment has evolved from 1990s Olympus BH-2 microscopes to 2025’s portable CytoViva Hyperspectral systems, which integrate fluorescence lifetime imaging for oxidative stress mapping. Session duration averages 35 minutes, with costs ranging from $120-$350 depending on follow-up consultations.
Observable Markers in Live Blood Test Analysis: What the Microscope Reveals
Under dark-field illumination, live blood test analysis highlights over 30 morphological and behavioral patterns validated in peer-reviewed studies. Red blood cell (RBC) flexibility appears as smooth, rapid flow in plasma streams; echinocytes (spiculated RBCs) indicate fatty acid imbalances or toxin exposure. Rouleaux stacks- coin-like RBC aggregates; correlate with elevated fibrinogen or dehydration, resolving within 72 hours of hydration in 68% of cases per a 2023 Journal of Orthomolecular Medicine trial.
White blood cell (WBC) activity shows neutrophils actively phagocytizing debris in infection or granulocytes exhibiting hyper-segmentation in B12 deficiency. Platelet aggregates signal hypercoagulability risks, while crystal formations (uric acid, cholesterol) suggest metabolic stress. Microbial elements- spirochetes, mycoplasma-like forms, or fungal hyphae- appear in chronic fatigue cohorts, though differentiation from artifacts requires phase-contrast confirmation.
A 2025 Microscopy Research and Technique study using confocal Raman spectroscopy validated 11 LBTA markers against serum biochemistry: RBC aggregation index matched ESR with r=0.89 correlation, and echinocyte percentage aligned with omega-3 index (r=0.82). These visual cues provide immediate biofeedback absent in static CBC reports.
Evidence-Based Benefits: Clinical Outcomes and Patient Engagement
Live blood test analysis delivers three primary advantages over conventional testing. First, immediacy: patients witness their blood in motion, increasing compliance with dietary interventions by 74% according to a 2024 Patient Education and Counseling randomized trial. Second, early detection of functional imbalances: rouleaux reversal after 30 days of anti-inflammatory protocols preceded CRP normalization by 6 weeks in 82 rheumatoid arthritis patients (2023 Rheumatology International). Third, personalization: visual patterns guide targeted supplementation-echinocytes resolving after 1 g/day EPA/DHA mirrored serum phospholipid improvements.
In diabetes management, live blood test analysis identifies erythrocyte rigidity linked to HbA1c >7.5%; a 2025 Diabetes Therapy pilot showed 64% of patients reduced A1c by 1.2 points after visualizing sugar-induced agglutination and adopting low-glycemic plans. For gastrointestinal health, fibrin strand density correlates with zonulin levels (r=0.76), prompting earlier gut-healing protocols. Wellness clinics report 40% of clients return for quarterly monitoring, creating longitudinal visual records absent in standard labs.
Accuracy and Validation: Comparing LBTA to Gold Standards
Critics argue that live blood test analysis lacks reproducibility, but controlled studies counter this. Inter-rater reliability among trained microscopists reaches 92% for rouleaux grading and 88% for echinocyte scoring using the Bradford Scale (0-4+). A 2025 Clinical Hemorheology and Microcirculation meta-analysis of 2,800 paired samples found:
- RBC aggregation index via LBTA vs. syllectometry: 89% concordance
- Platelet aggregation visualization vs. light transmission aggregometry: 85% sensitivity
- WBC activation (rolling/adhesion) vs. flow cytometry CD11b expression: 81% specificity
Artifacts: air bubbles, drying edges, or cholesterol droplets; mimic pathogens in 3-5% of fields but are excluded via time-lapse confirmation. FDA does not regulate LBTA as a diagnostic device since it is observational, not quantitative; however, CLIA-waived microscopes must meet ISO 15189 quality standards for image calibration.

Clinical Integration: How Practitioners Use Live Blood Test Analysis
Functional medicine clinics embed live blood test analysis within multi-modal assessments. A typical workflow begins with symptom questionnaires and serum panels, followed by LBTA as a visual bridge. Findings trigger reflex testing: persistent rouleaux prompt D-dimer and homocysteine; spicule formation leads to RBC fatty acid profiles.
In sports medicine, live blood test analysis monitors overtraining; poikilocyte spikes after intense sessions resolve with a 48-hour recovery, guiding periodization. Pediatric naturopaths use LBTA to visualize dairy-induced agglutination, motivating elimination diets with 78% parental adherence. Corporate wellness programs deploy mobile LBTA units; a 2025 Google Health pilot reduced employee sick days by 22% after visualizing dehydration patterns and implementing hydration challenges.
Telemedicine integration allows remote viewing: patients prick at home, stream via 5G-enabled microscopes, and receive narrated sessions. HIPAA-compliant platforms like MicroHealth Live store encrypted 4K videos for longitudinal comparison.
Regulatory Landscape and Ethical Practice Standards
Live blood test analysis operates in a regulatory gray zone. The FDA classifies dark-field microscopes as Class I devices for general microscopy, not diagnostics. Practitioners cannot claim disease diagnosis; language must remain observational: “appears consistent with oxidative stress” rather than “indicates diabetes.” The IALBA mandates 120-hour certification, annual proficiency, and informed consent disclosing LBTA’s complementary status.
Malpractice risks arise from over-interpretation; a 2024 California case awarded $180,000 after a practitioner misidentified cholesterol crystals as parasites. Ethical guidelines require referral to MDs for abnormal findings warranting medical intervention, e.g., target cells prompting hemoglobin electrophoresis.
Case Studies: Real-World Transformations via Live Blood Test Analysis
Case 1: Chronic Fatigue Resolution (Toronto Functional Clinic, 2025)
A 42-year-old teacher presented with 18-month fatigue. Baseline live blood test analysis showed 3+ rouleaux, echinocytes, and fibrin mesh. Serum revealed ferritin 18 ng/mL and CRP 4.2 mg/L. Interventions: 40 mg iron bisglycinate daily, 2 g omega-3, and hydration protocol. Week 4 LBTA: rouleaux dissolved, echinocytes reduced 70%. Week 12: energy restored, ferritin 78 ng/mL, CRP 0.9 mg/L.
Case 2: Athletic Performance Optimization (U.S. Olympic Training Center, 2024)
A cyclist exhibited 2+ platelet aggregates post-altitude camp. Live blood test analysis guided beetroot supplementation and L-citrulline; aggregates cleared in 72 hours, correlating with 8% VO2 max improvement.
Case 3: Pediatric Allergy Management (Sydney Naturopathic Practice, 2025)
A 6-year-old with eczema showed dairy-induced RBC clumping. Elimination diet plus probiotics normalized the blood picture in 21 days; skin cleared 85%, validated by SCORAD reduction.
From X (Oct 2025): @FunctionalDoc posted a before/after LBTA video of rouleaux dissolving after 30 days keto; caption: “Patient saw the stacks vanish, now down 28 lbs.”

Technological Advancements: AI and Automation in LBTA
2025 ushers in AI augmentation. DeepLens AI overlays machine learning on live feeds, auto-flagging echinocytes with 96% sensitivity and quantifying aggregation indices in 3 seconds. HoloMicroscope AR systems project 3D blood models onto practitioner goggles for immersive client education.
Portable units like CellScope Pro weigh 1.2 kg, connect via USB-C, and run on solar chargers for field use in rural India. Hyperspectral imaging differentiates hemoglobin oxygenation states, revealing tissue perfusion deficits invisible in standard microscopy.
Challenges and Limitations: Addressing the Critics
Live blood test analysis faces four core criticisms. Subjectivity: mitigated via standardized scoring and AI calibration. Lack of quantitative output: addressed by hybrid protocols pairing LBTA with serum markers. Artifact confusion: reduced through time-lapse and phase-contrast toggling. Evidence gaps: ongoing RCTs like the 2026–2028 NIH-funded trial comparing LBTA-guided vs. standard interventions in metabolic syndrome.
Cost and accessibility limit mainstream adoption; insurance rarely covers LBTA, positioning it as out-of-pocket wellness spending.
Future Directions: From Observation to Predictive Modeling
By 2030, live blood test analysis will be integrated with wearable biosensors. Continuous microfluidic patches feed micro-droplets to bedside scopes, enabling 24/7 monitoring. Machine learning models trained on 1 million LBTA frames predict cardiovascular events 30 days earlier than CRP trends.
Global standardization via the World Naturopathic Federation will establish reference atlases. Blockchain-secured image repositories ensure longitudinal integrity for clinical trials.
Conclusion
Live blood test analysis transforms a routine finger prick into a cinematic window on health, revealing dynamic imbalances that static labs miss. Its benefits, immediate visual motivation, early functional detection, and personalized interventions, are substantiated by clinical outcomes and patient engagement metrics. Accuracy, when performed under controlled conditions with trained observers, rivals traditional hemorheology for key markers.
While not a replacement for conventional diagnostics, live blood test analysis serves as a powerful adjunct in functional medicine, sports performance, and preventive wellness. Practitioners must adhere to ethical boundaries, refer appropriately, and leverage emerging AI tools. For patients, seeing is believing: the moment rouleaux dissolve or echinocytes smooth out often marks the turning point from symptom management to true vitality. In an era craving tangible health insights, live blood test analysis offers exactly that; one living drop at a time.