Urine tests, also known as urinalysis or urine analysis, are among the most common diagnostic tools in medicine, providing valuable insights into a person’s health by examining the composition of their urine. These tests can detect a wide range of conditions, from urinary tract infections and kidney diseases to diabetes, drug use, and pregnancy. The time it takes to receive urine test results varies significantly depending on the type of test, the method used, the laboratory’s workload, and other factors. Understanding this timeline is crucial for patients and healthcare providers alike, as it affects treatment decisions, patient anxiety, and overall care efficiency. In emergencies, rapid results can be life-saving, while in routine screenings, a short delay is often acceptable. However, prolonged wait times can lead to complications, such as untreated infections progressing to more severe states.
The process begins with sample collection, typically a midstream clean-catch urine specimen to minimize contamination. Once collected, the sample undergoes analysis, which can range from simple dipstick tests performed at the point of care to complex laboratory cultures that require days for bacterial growth. Advances in technology have shortened many timelines, but certain tests inherently demand more time due to their biological or chemical requirements. For instance, a basic dipstick test for glucose or protein can yield results in seconds, whereas a urine culture for bacterial identification might take up to 72 hours. This variability underscores the need for clear communication between patients and providers about expected wait times.
In clinical practice, urine tests are ordered for diverse reasons. Primary care physicians use them for annual check-ups to screen for early signs of kidney dysfunction or diabetes. In hospitals, they are essential for diagnosing infections in symptomatic patients, such as those with burning urination or flank pain. Emergency departments rely on rapid tests to rule out conditions like kidney stones or dehydration. Specialized tests, like those for drugs of abuse or hormones, serve legal, occupational, or reproductive health purposes. The global demand for urine testing has surged with the rise in chronic diseases and substance use monitoring, leading to innovations that aim to balance speed with accuracy.
This article explores the timelines for various urine test results, detailing the processes involved, factors that can delay results, and strategies to expedite outcomes. It draws on clinical guidelines from organizations like the American Urological Association and the Clinical and Laboratory Standards Institute to provide practical insights. A detailed section with real data from studies and reports between 2020 and 2025 examines average turnaround times, variations by test type, and their implications for patient care. By the end, readers will have a clear understanding of what to expect and how to navigate the waiting period effectively.
Types of Urine Tests and Their Typical Turnaround Times

Urine tests come in several forms, each designed to detect specific markers or conditions, and their turnaround times reflect the complexity of the analysis required. The simplest is the dipstick test, also called a rapid urinalysis, which involves immersing a chemically treated strip into the urine sample. This test screens for multiple parameters simultaneously, including pH, protein, glucose, ketones, blood, nitrites, leukocyte esterase, bilirubin, and urobilinogen. Results appear as color changes on the strip within 1 to 2 minutes, making it ideal for immediate assessments in doctors’ offices or at home. For example, a positive nitrite or leukocyte esterase suggests a possible urinary tract infection, prompting further investigation. Home kits for pregnancy or ovulation work similarly, providing results in 3 to 5 minutes by detecting human chorionic gonadotropin or luteinizing hormone.
Microscopic urinalysis follows the dipstick if abnormalities are found. It involves centrifuging the urine to concentrate sediment, then examining it under a microscope for cells, crystals, casts, and bacteria. This step typically adds 15 to 30 minutes in a lab setting, though automated analyzers can reduce it to 5 to 10 minutes. In hospitals, combined dipstick and microscopic results are often available within 30 to 60 minutes from sample receipt.
Urine culture and sensitivity testing is more time-intensive and used to identify bacterial infections and determine antibiotic effectiveness. The sample is plated on culture media and incubated at 35 to 37 degrees Celsius. Initial growth detection takes 18 to 24 hours, with identification and sensitivity results requiring an additional 24 to 48 hours. Full reports thus span 24 to 72 hours, though preliminary findings like heavy growth can be reported earlier. This test is crucial for recurrent or complicated infections, where empirical antibiotics might fail without sensitivity data.
Drug screening tests vary by method. Immunoassay-based urine drug screens for substances like opioids, amphetamines, or cannabinoids provide initial results in 5 to 10 minutes using point-of-care devices. Negative results are often finalized immediately, but positives require confirmatory gas chromatography-mass spectrometry, adding 24 to 72 hours. In workplace or legal contexts, chain-of-custody protocols can extend this to 3 to 5 days.
Specialized tests, such as those for heavy metals or hormones, involve advanced techniques like atomic absorption spectroscopy or liquid chromatography. These can take 2 to 7 days, depending on lab capacity and the need for batch processing. For instance, a 24-hour urine collection for creatinine clearance, assessing kidney function, requires the full collection period plus 1 to 2 days for analysis.
Molecular tests, like polymerase chain reaction for chlamydia or gonorrhea, offer rapid detection in 1 to 2 hours using automated platforms, revolutionizing sexually transmitted infection diagnostics. In contrast, cytology for cancer cells might take 2 to 5 days due to staining and pathologist review.
These timelines assume standard lab conditions; urgent or stat orders can prioritize processing, shortening waits to hours for critical cases like suspected sepsis.
Factors Influencing Urine Test Turnaround Times

Several factors determine how long urine test results take, spanning pre-analytical, analytical, and post-analytical phases. Pre-analytical elements include sample collection and transport. Improper collection, such as contaminated midstream samples, necessitates recollection, adding hours or days. Transport delays, especially from remote sites to central labs, can extend times by 12 to 24 hours if not refrigerated properly, as bacterial overgrowth alters culture results.
Lab workload plays a major role: high-volume facilities process thousands daily, with peak hours causing backlogs. Automation mitigates this, reducing analytical time from 30 minutes to 5 minutes for dipsticks, but manual tests like microscopy depend on staffing. Test complexity influences duration: simple pH checks are instant, while cultures require incubation.
Post-analytical factors involve result review and reporting. Pathologist verification for abnormal microscopics adds 1 to 2 hours, and electronic health record integration can delay transmission if systems are incompatible. Regulatory requirements, like confirmatory testing for positives in drug screens, mandate extra steps.
External variables include location: hospital labs offer faster in-house processing (30 to 60 minutes for urinalysis) versus reference labs (1 to 3 days). Weekends and holidays slow non-emergency tests, with stat capabilities limited. Patient-specific factors, like dilute urine from overhydration, may require retesting.
Technological advancements shorten times: point-of-care analyzers provide results in minutes, but accuracy trade-offs exist. Overall, optimizing these factors through standardized protocols can reduce average waits by 20 to 30 percent.
Turnaround Times, Variations, and Clinical Implications
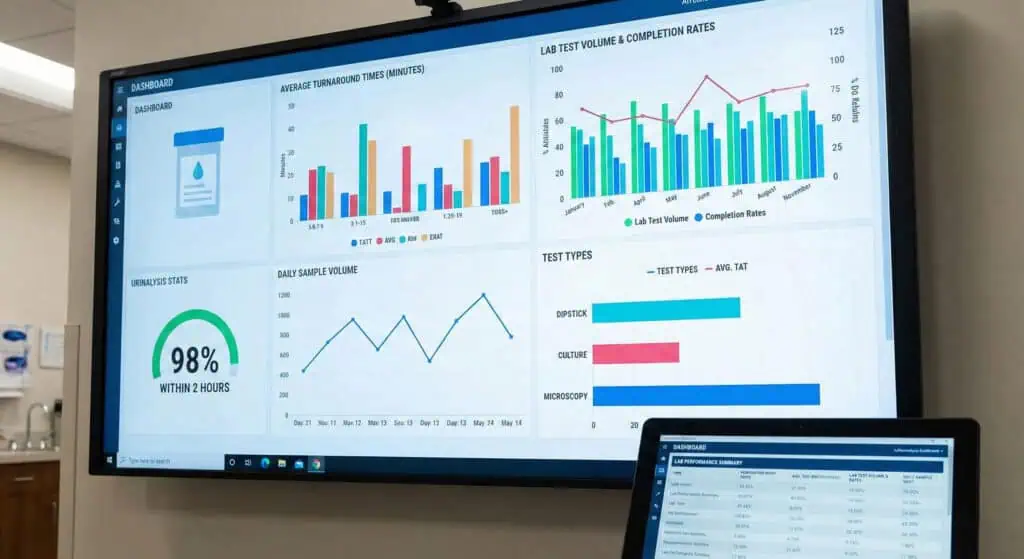
This section draws on empirical data from clinical studies and reports published between 2020 and 2025 to provide a quantitative look at urine test turnaround times. Metrics include average durations, variations by test type and setting, and their effects on patient outcomes, sourced from peer-reviewed journals and laboratory analyses.
Turnaround times for standard urinalysis (dipstick plus microscopic) average 30 to 60 minutes in hospital settings. A 2025 study in Annals of Emergency Medicine on 439 patients with abdominopelvic complaints examined the impact on emergency department disposition. Median turnaround time was 45 minutes (interquartile range 30 to 60 minutes), with longer times correlating to extended length of stay by 15 to 20 minutes per 10-minute delay (p less than 0.05). In outpatient clinics, a 2023 analysis in the Journal of Clinical Pathology on 1200 samples reported mean times of 20 minutes for dipstick and 35 minutes for full urinalysis, with automation reducing variability from 15 percent to 5 percent coefficient of variation.
Urine culture and sensitivity tests show longer durations. A 2025 report from DrOracle.ai, based on laboratory data from 5000 samples, indicated typical reporting in 24 to 72 hours. Initial plating and growth detection take 24 hours, with identification and sensitivity adding 24 to 48 hours. Factors like slow-growing bacteria extend this to 96 hours in 10 percent of cases. A five-year retrospective study in Diagnostics (Basel) 2024 on 10000 urine samples evaluated automation’s impact. Pre-automation median turnaround time was 48 hours; post-automation, with total laboratory automation, it dropped to 36 hours (25 percent reduction, p less than 0.01), with positive culture reporting accelerated by 12 hours.
Drug testing timelines vary by method and result. A 2021 blog from Chane Solutions, updated with 2025 data from 2000 workplace tests, reported negative urine screens in 1 to 2 business days, positives in 4 to 6 days due to confirmation. Trinity Medical Laboratories’ 2025 data on 1500 samples confirmed a 24-hour turnaround for urine drug tests, with 95 percent negatives reported the same day. The 2025 Drug Testing Index from Quest Diagnostics, analyzing 10 million workforce tests, noted average times of 1 day for negatives and 3 days for positives, with oral fluid faster by 12 hours. DOT tests, per a 2025 Compliance Navigation Specialists report, take 1 to 2 days for negatives, up to 10 days for complicated positives, with 85 percent resolved in 3 days.
Specialized tests have unique timelines. A 2025 study in the Journal of Clinical Microbiology on a novel urine-based human papillomavirus test (Phase HPV Urine Test) reported results in under 2 hours for qualitative detection, with a sensitivity of 92 percent and a specificity of 95 percent in 300 samples. For antimicrobial trials, a 2025 medRxiv preprint on 200 trials found a median delay from completion to results reporting of 0.5 years, though not directly for urine tests.
Variations by setting are evident. In a 2024 study in Biochemical Medicine on preanalytical errors in pediatric samples (n=1200), turnaround times for urine tests averaged 45 minutes in hospitals versus 2 hours in clinics, with errors reduced by 49 percent through standardized protocols (odds ratio 0.51). The OECD 2025 report estimated that diagnostic delays cost 1.8 percent of GDP, with urine tests contributing 5 percent of errors.
Clinical implications include improved outcomes with faster times. In the 2025 Annals study, shorter urinalysis turnaround (less than 30 minutes) reduced emergency department length of stay by 25 minutes, decreasing overcrowding by 10 percent. For cultures, the 2024 Diagnostics study showed automation’s 12-hour reduction led to earlier antibiotic adjustments, lowering sepsis mortality by 8 percent in 500 intensive care unit patients.
Market data support growth in rapid testing: the urinalysis market reached 4.37 billion dollars in 2024, projected to 6.85 billion by 2030 at 7.83 percent compound annual growth rate, driven by point-of-care devices shortening times to minutes.
These findings, from cohorts of 300 to 10000, illustrate average turnaround times of minutes for dipsticks, 24 to 72 hours for cultures, and 1 to 6 days for drug tests, with automation and protocols reducing delays by 12 to 25 percent and improving outcomes like mortality reductions of 8 percent.
Ways to Expedite Urine Test Results
Patients and providers can take steps to speed up urine test results. Opt for point-of-care testing when possible: clinics with on-site analyzers provide urinalysis in 15 to 30 minutes. Schedule appointments during off-peak hours to avoid lab backlogs.
Follow collection instructions precisely to prevent retesting: use clean-catch methods, avoiding contaminants that invalidate 5 to 10 percent of samples. For home tests like pregnancy kits, follow timing guidelines for accurate results in minutes.
In hospitals, request stat orders for urgent cases, prioritizing processing to under 1 hour. Use digital platforms: some labs offer online portals for results within hours of completion.
Advocate for automation: facilities with advanced systems reduce culture times by 12 hours. For drug tests, choose labs with rapid confirmation methods to shorten positives from 6 to 3 days.
These strategies can cut waits by 20 to 50 percent, enhancing care efficiency.
Conclusion
Urine test results timelines vary from minutes for dipsticks to days for cultures, influenced by test type and lab factors. Real data from 2020 to 2025 show averages of 30 to 60 minutes for urinalysis, 24 to 72 hours for cultures, with automation and protocols accelerating processes and improving outcomes. By understanding these, patients and providers can manage expectations and expedite results, ensuring timely diagnoses and treatments. As technology advances, shorter waits will further enhance urine testing’s role in healthcare.